The doctor will see you now, with a little help from AI

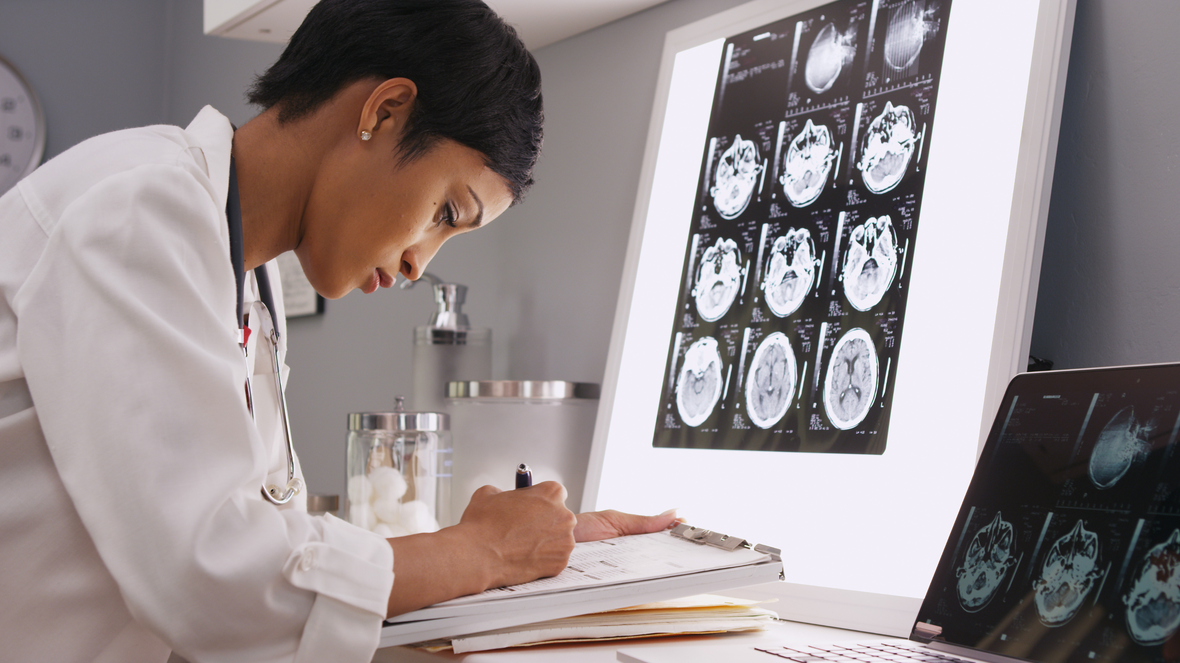
A few years ago, a radiologist sat in a dimly lit room, her eyes scanning a series of black and white images on a high-resolution screen. It was a familiar routine. She was looking for the subtle shadows and faint patterns that could signal a developing tumor in a patient's lung scan. This time, however, something was different. A small, color-coded box, overlaid by a new software program, was highlighting a tiny region she might have otherwise passed over.
The software was not making a diagnosis. It was simply pointing, whispering a digital “what about here?” The radiologist, with her years of training and experience, made the final call. But that small nudge, that computational second opinion, represents a quiet but profound shift happening in medicine. It’s a shift powered by artificial intelligence.
When we think of AI, our minds often drift to science fiction or self-driving cars. The reality of its application in healthcare is far more grounded and, in many ways, more impactful. It is not about replacing doctors but about augmenting their abilities, giving them tools to see more clearly, understand more deeply, and act more precisely than ever before.
This technology is steadily weaving itself into the fabric of diagnostics, drug discovery, personalized medicine, and daily patient care. It is a complex and fascinating evolution, one that deserves a closer look beyond the headlines and hype.
Seeing the unseen in medical diagnostics
One of the most mature and compelling uses of AI in healthcare is in medical imaging. Radiologists, pathologists, and dermatologists are experts in pattern recognition. They spend years learning to identify abnormalities in X-rays, CT scans, MRIs, and tissue samples. Yet, the task is demanding, and the sheer volume of data can be immense.
This is where AI, specifically a type of machine learning called deep learning, comes into play. These algorithms are trained on vast datasets of labeled images. They learn to identify the telltale signs of diseases like cancer, diabetic retinopathy, or stroke with remarkable accuracy.
Think of it like teaching a child to recognize a cat. You show them thousands of pictures of cats of all shapes, sizes, and colors. Eventually, they learn the underlying patterns and can identify a cat they have never seen before. AI models learn in a similar way, but instead of cats, they learn to spot malignant cells or blocked arteries.
In practice, this does not mean an AI makes the final diagnosis. Instead, it acts as a tireless assistant. It can triage cases, flagging the most urgent scans for immediate review. It can highlight suspicious areas on an image, drawing the clinician's attention to subtle details that might be missed during a long shift. This collaboration between human expertise and machine precision promises to make diagnostics faster, more accurate, and more accessible.

The applications extend beyond just cancer detection. AI algorithms are now helping to identify early signs of eye diseases that can lead to blindness by analyzing retinal scans. They are also being used in cardiology to analyze echocardiograms, helping to detect heart conditions that could otherwise go unnoticed until they become critical.
This isn't about an algorithm outperforming a doctor. It's about a doctor empowered by an algorithm becoming better than a doctor alone. The goal is to reduce diagnostic errors, catch diseases earlier, and ultimately give patients a better chance at a successful outcome.
Accelerating the search for new medicines
Discovering a new drug is a long, expensive, and often frustrating process. It can take more than a decade and cost billions of dollars to bring a single new medicine to market. For every success story, there are thousands of promising compounds that fail somewhere along the arduous path of research and clinical trials.
AI is beginning to change this equation by dramatically speeding up the earliest stages of drug discovery. One of the biggest challenges is identifying a viable "target," such as a specific protein involved in a disease, and then finding a molecule that can interact with that target to produce a therapeutic effect.
Traditionally, this has been a process of painstaking trial and error. AI can sift through massive biological and chemical datasets at a speed no human could ever match. It can analyze genetic information, protein structures, and patient data to identify promising new drug targets.
Once a target is identified, AI can then predict which molecules are most likely to bind to it effectively. It can simulate how a potential drug will behave in the human body, helping researchers prioritize the most promising candidates for further testing. This computational approach saves immense amounts of time and resources, allowing scientists to focus their efforts where they are most likely to succeed.
For example, AI models can analyze the intricate, three-dimensional shapes of proteins, which is crucial for designing drugs that fit into them like a key in a lock. What used to take months or years of lab work can now be modeled in a matter of hours or days. This is not just an incremental improvement. It is a fundamental change in the way we approach the science of medicine creation.
This acceleration is already having an impact. AI-powered platforms have helped identify novel drug candidates for conditions ranging from neurological disorders to infectious diseases. While these candidates still have to go through rigorous clinical trials, getting to that stage faster means that potentially life-saving treatments could reach patients years earlier than they would have otherwise.
Medicine tailored to you
For much of modern medical history, treatment has followed a one-size-fits-all model. A diagnosis would lead to a standard course of treatment that worked for many people but not for everyone. The concept of personalized medicine, or precision medicine, aims to change that by tailoring medical decisions and treatments to the individual characteristics of each patient.
AI is the engine that makes this level of personalization possible. Our bodies are incredibly complex systems, and how we respond to a disease or a treatment is influenced by our unique genetics, lifestyle, and environment. AI can analyze this vast and varied data to uncover patterns that would be invisible to a human observer.
Consider cancer treatment. Two patients might have the same type of cancer, but the specific genetic mutations driving their tumors could be very different. An AI system can analyze the genomic data from a patient's tumor and compare it to a massive database of clinical information.
This analysis can help predict which specific chemotherapy drug or targeted therapy is most likely to be effective for that individual patient. It can also help identify patients who might benefit from a particular clinical trial. This moves treatment away from a trial-and-error approach and toward a more targeted, data-driven strategy.
This personalization extends beyond just treatment selection. AI can also help predict a patient's risk of developing certain diseases. By analyzing electronic health records, genetic information, and even data from wearable devices, algorithms can identify individuals who are at high risk for conditions like heart disease or diabetes.
This allows for proactive interventions. A doctor could recommend specific lifestyle changes or more frequent screenings for a patient identified as high-risk, potentially preventing the disease from ever developing. It is a shift from reactive to preventive healthcare, all made possible by the ability to make sense of deeply personal health data.


A constant companion in patient care
The role of AI in healthcare is not confined to the hospital or the research lab. It is also becoming an increasingly important part of ongoing patient care and management, especially for those with chronic conditions. Managing a disease like diabetes, for example, requires constant monitoring and small adjustments throughout the day.
AI-powered tools are helping to ease this burden. Smart glucose monitors can connect with apps that use AI to predict how a patient's blood sugar levels will change based on their diet, exercise, and insulin intake. This helps patients make better decisions and avoid dangerous highs and lows.
Virtual health assistants and chatbots are another growing area. These AI-powered tools can answer patient questions, provide medication reminders, and help individuals track their symptoms. This provides patients with 24/7 support and can help free up clinicians' time to focus on more complex cases.
These are not meant to replace conversations with nurses or doctors. Instead, they serve as a helpful first line of support, managing routine tasks and ensuring patients feel connected to their care plan even when they are at home.
AI is also playing a role in the administrative side of healthcare. It can help automate tasks like scheduling appointments, managing medical records, and processing insurance claims. While less glamorous than drug discovery, reducing this administrative burden is crucial. It gives doctors and nurses more time to do what they do best: care for patients.
This more efficient, supportive, and continuous model of care helps bridge the gaps between hospital visits. It empowers patients to take a more active role in managing their own health and ensures that care teams have a more complete picture of a patient's well-being over time.
The road ahead is paved with questions
The potential of AI in healthcare is immense, but it is not without its challenges and important ethical questions. One of the biggest concerns is data privacy. Medical data is incredibly sensitive, and ensuring it is used securely and responsibly is paramount. We need robust regulations and transparent policies to build and maintain public trust.
Another critical issue is bias. AI models are only as good as the data they are trained on. If the training data is not diverse and representative of the entire population, the resulting algorithms can perpetuate and even amplify existing health disparities. For an AI tool to be fair and effective for everyone, it must be trained on data from people of all races, ethnicities, and backgrounds.
There is also the question of accountability. If an AI system contributes to a misdiagnosis, who is responsible? Is it the doctor who used the tool, the hospital that implemented it, or the company that developed it? These are complex legal and ethical questions that we are only just beginning to navigate.
Finally, we must never lose sight of the human element in medicine. A doctor's empathy, intuition, and ability to communicate with a patient are irreplaceable. AI should always be seen as a tool to support, not supplant, the vital relationship between a patient and their caregiver. The goal is to enhance human connection in healthcare, not automate it away.


A tool, not a cure-all
The story of AI in healthcare is not one of a technological revolution that will instantly solve all of our problems. It is a story of steady, thoughtful integration. It is about building better tools that help dedicated professionals do their jobs more effectively.
That radiologist looking at the screen is still the expert. Her judgment and experience remain the most critical part of the diagnostic process. The AI is simply a new kind of stethoscope or a more advanced microscope. It allows her to perceive things she could not before, augmenting her natural abilities with the power of computation.
From finding subtle clues in a medical scan to accelerating the search for a life-saving drug, AI is quietly becoming an indispensable partner in medicine. It is a collaboration between human intelligence and artificial intelligence, working together to create a future where healthcare is more precise, more personal, and more effective for us all.
Related articles
You deserve a better browser


Press Contacts!
Our press team loves working with journalists from around the world. If you’re a member of the media and would like to talk, please get in touch with us by sending an email to one of our team members or to press-team@opera.com